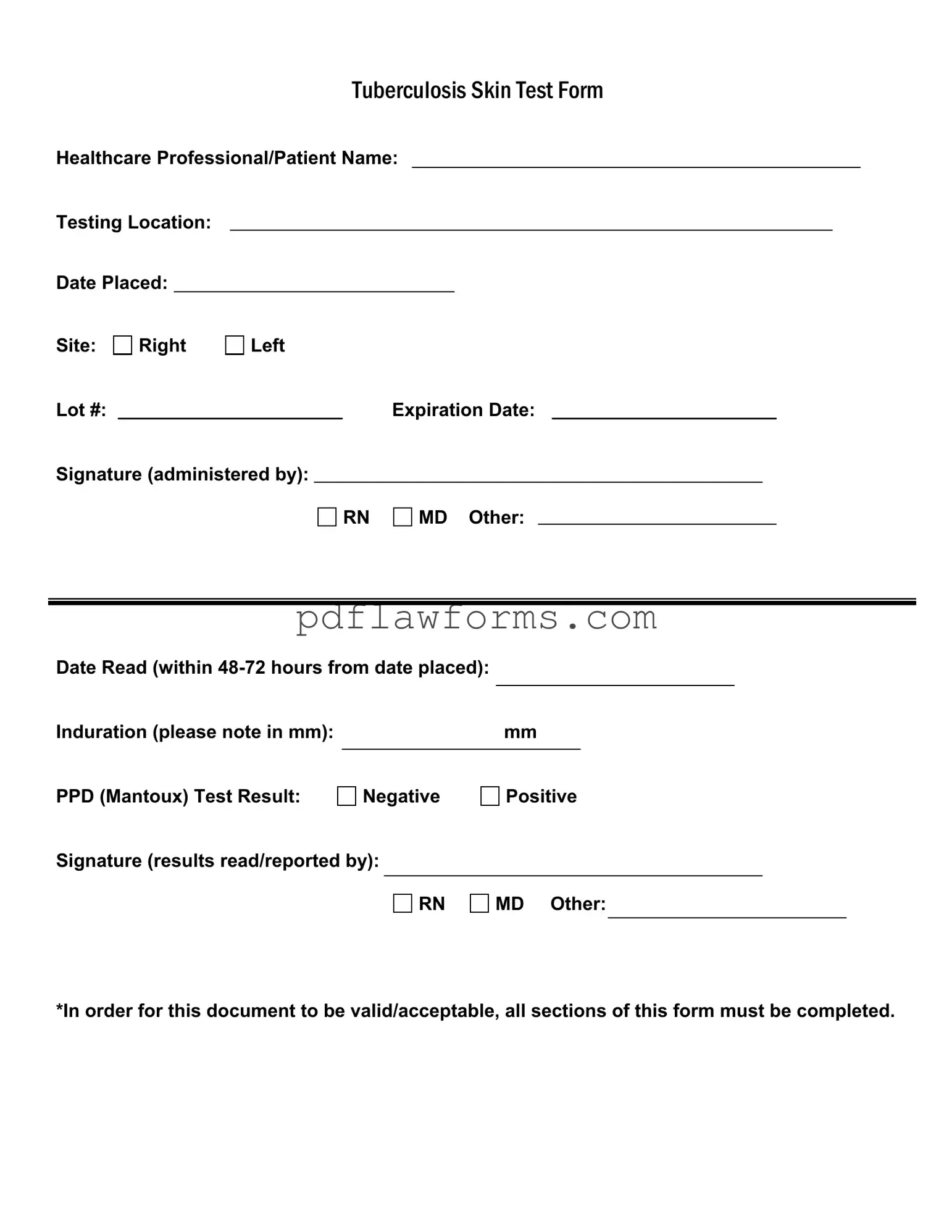
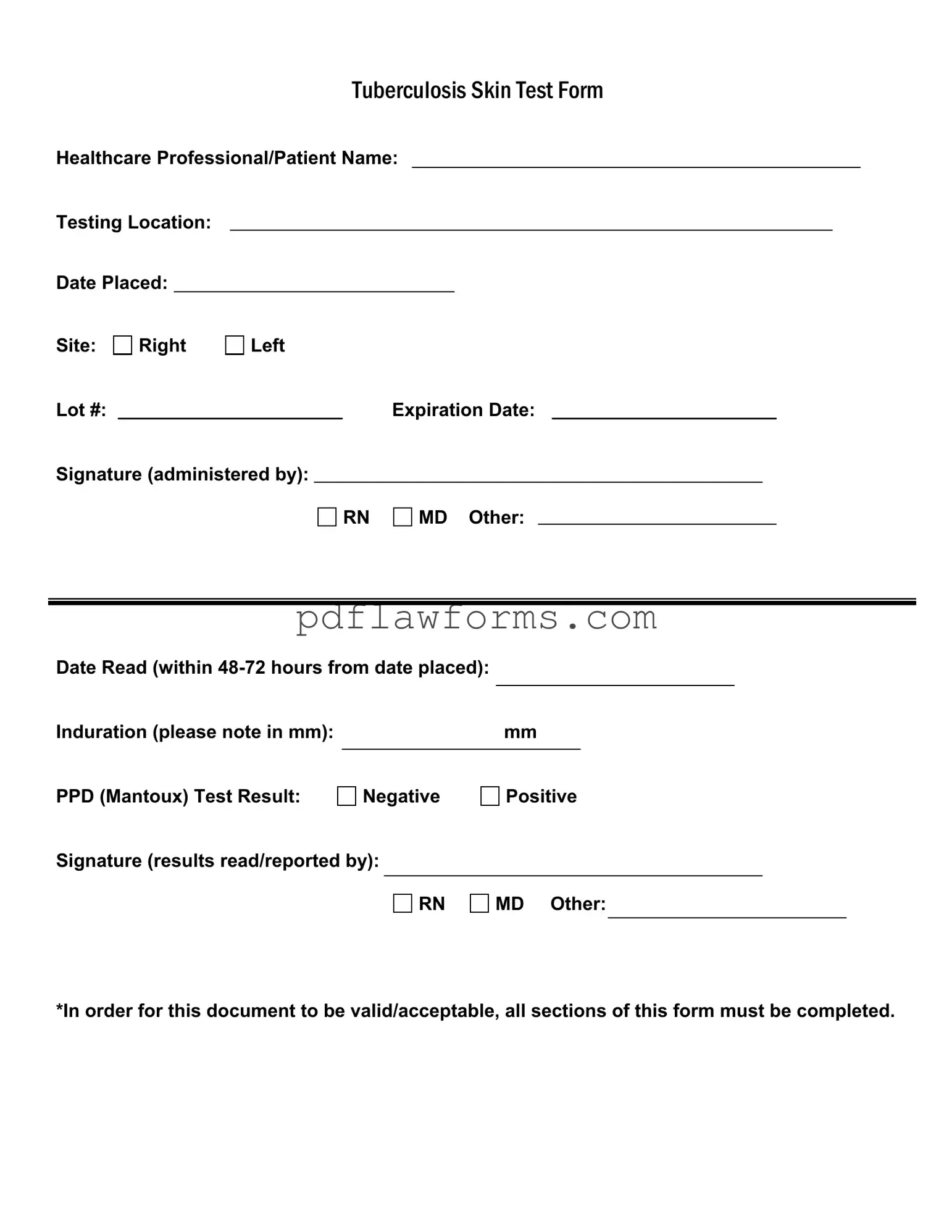
Filling out the Tuberculosis (TB) Skin Test form accurately is essential for ensuring that the results are valid and that the individual receives appropriate care. One common mistake is failing to complete all required sections of the form. Every part of the document is important, and omitting even a single detail can lead to complications in processing the test results.
Another frequent error involves not providing the correct dates. The form requires the date the test was placed as well as the date it was read. If these dates are incorrect or missing, it can create confusion regarding the timing of the test and its validity. It is crucial to double-check that these dates align with the testing timeline.
Many individuals also overlook the importance of noting the site of the test placement. The form specifies whether the test was administered on the right or left arm. Failure to indicate this can lead to difficulties in interpreting the results, especially if there is a need for follow-up testing.
Inaccurate measurement of induration is another common mistake. The form asks for the size of the induration in millimeters. If this measurement is not taken correctly, it could lead to an incorrect interpretation of the test result. It is important to measure the induration accurately and record it clearly on the form.
Some people may forget to include the lot number and expiration date of the PPD (Purified Protein Derivative) used for the test. This information is critical for tracking the test's validity and ensuring that the materials used were not expired. Omitting these details can compromise the integrity of the test.
Providing an incorrect test result is another issue that can arise. The form has a section for indicating whether the PPD test result is negative or positive. Misreporting this result can lead to unnecessary anxiety or, conversely, a lack of necessary follow-up care. It is vital to ensure that the result is accurately reflected on the form.
Signatures are required from both the healthcare professional administering the test and the individual reading the results. Some individuals may forget to sign the form, which can render it invalid. Both signatures are essential for confirming that the test was conducted and interpreted properly.
Another mistake involves not adhering to the time frame for reading the test results. The form states that the test must be read within 48 to 72 hours after placement. If the results are not read within this window, the test may need to be repeated, leading to delays in diagnosis or treatment.
Lastly, individuals sometimes fail to communicate any prior history of TB or related health issues. This information is important for healthcare providers to consider when interpreting the results. Being thorough in this section can help ensure that the individual receives the most appropriate care based on their medical history.