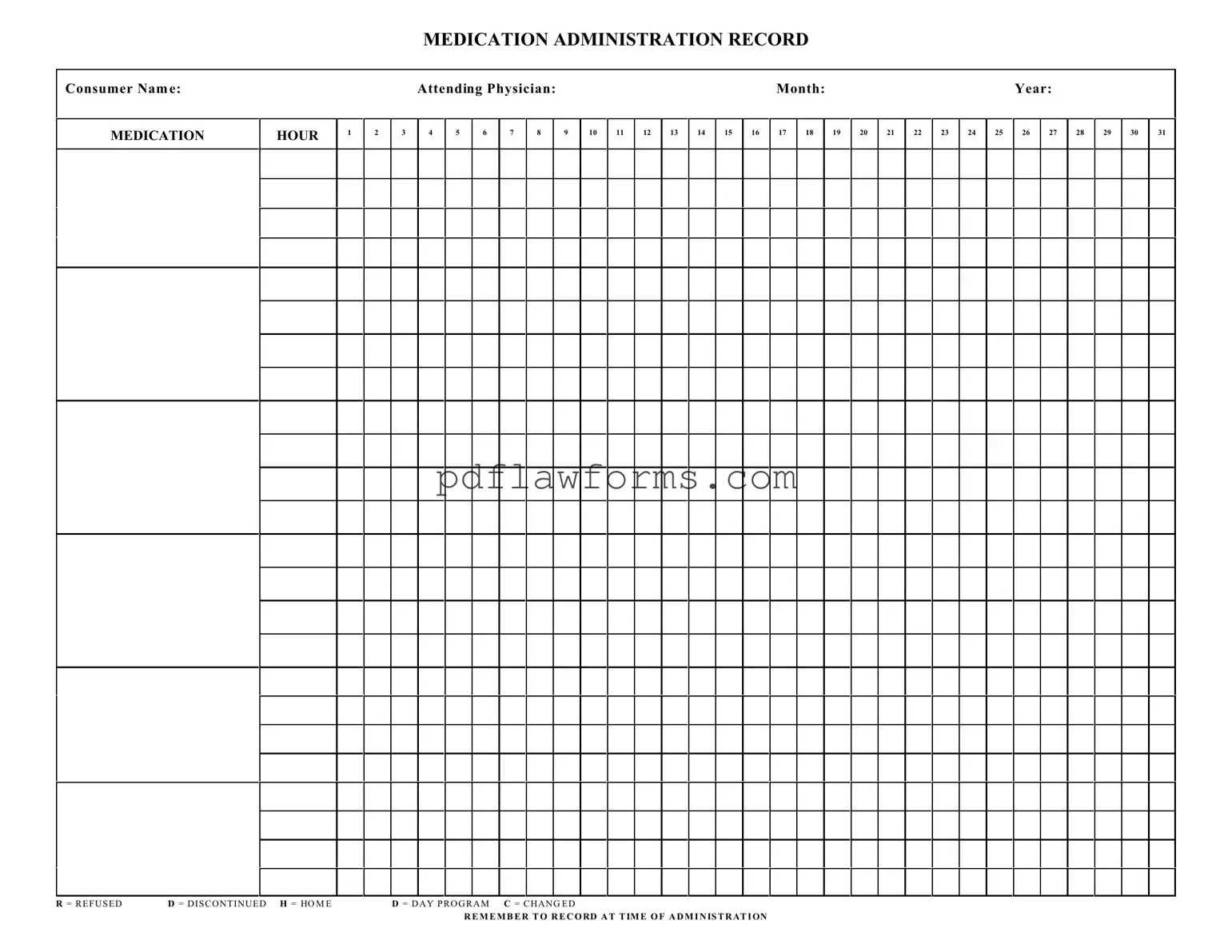
Fill Your Medication Administration Record Sheet Template
The Medication Administration Record Sheet is a crucial tool used to track the administration of medications to patients. This form helps ensure that medications are given accurately and on time, promoting patient safety and effective care. To start using the form, click the button below to fill it out.
Make My Document Online
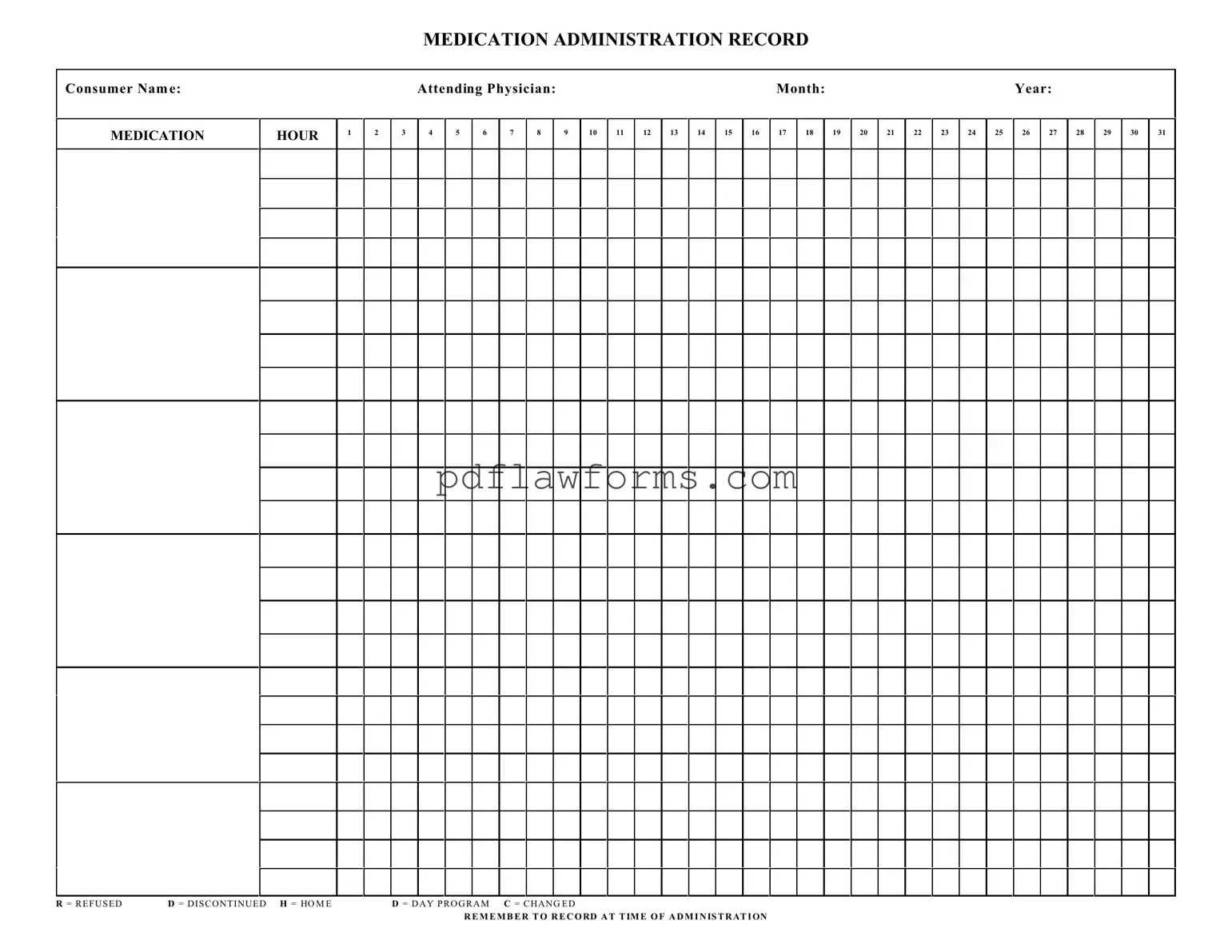
Fill Your Medication Administration Record Sheet Template
Make My Document Online
You’re halfway through — finish the form
Edit and complete Medication Administration Record Sheet online, then download your file.
Make My Document Online
or
⇩ Medication Administration Record Sheet PDF