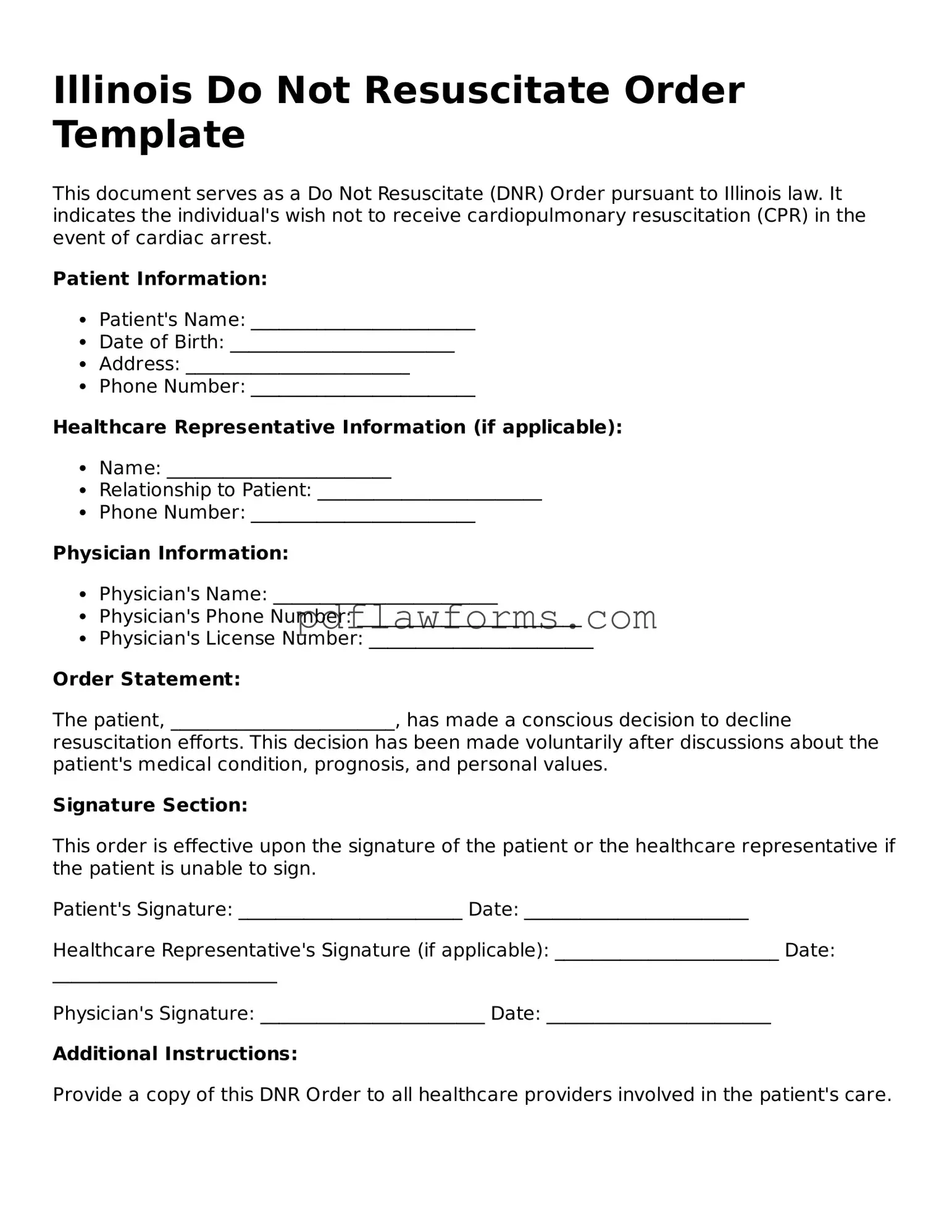
Do Not Resuscitate Order Form for the State of Illinois
A Do Not Resuscitate (DNR) Order in Illinois is a legal document that allows individuals to refuse resuscitation efforts in the event of a medical emergency. This form is crucial for those who wish to ensure their end-of-life wishes are respected. To take control of your healthcare decisions, consider filling out the DNR Order form by clicking the button below.
Make My Document Online
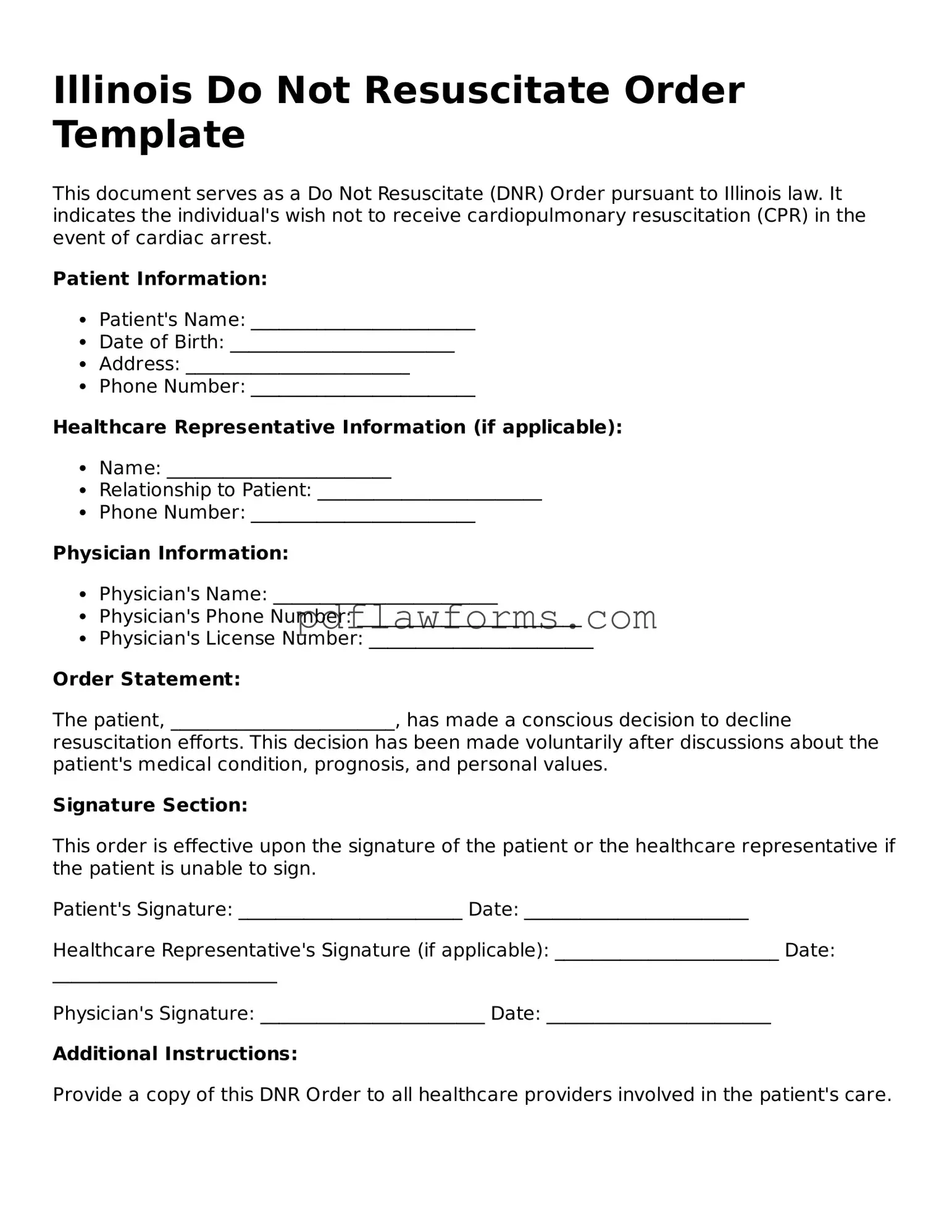
Do Not Resuscitate Order Form for the State of Illinois
Make My Document Online
You’re halfway through — finish the form
Edit and complete Do Not Resuscitate Order online, then download your file.
Make My Document Online
or
⇩ Do Not Resuscitate Order PDF