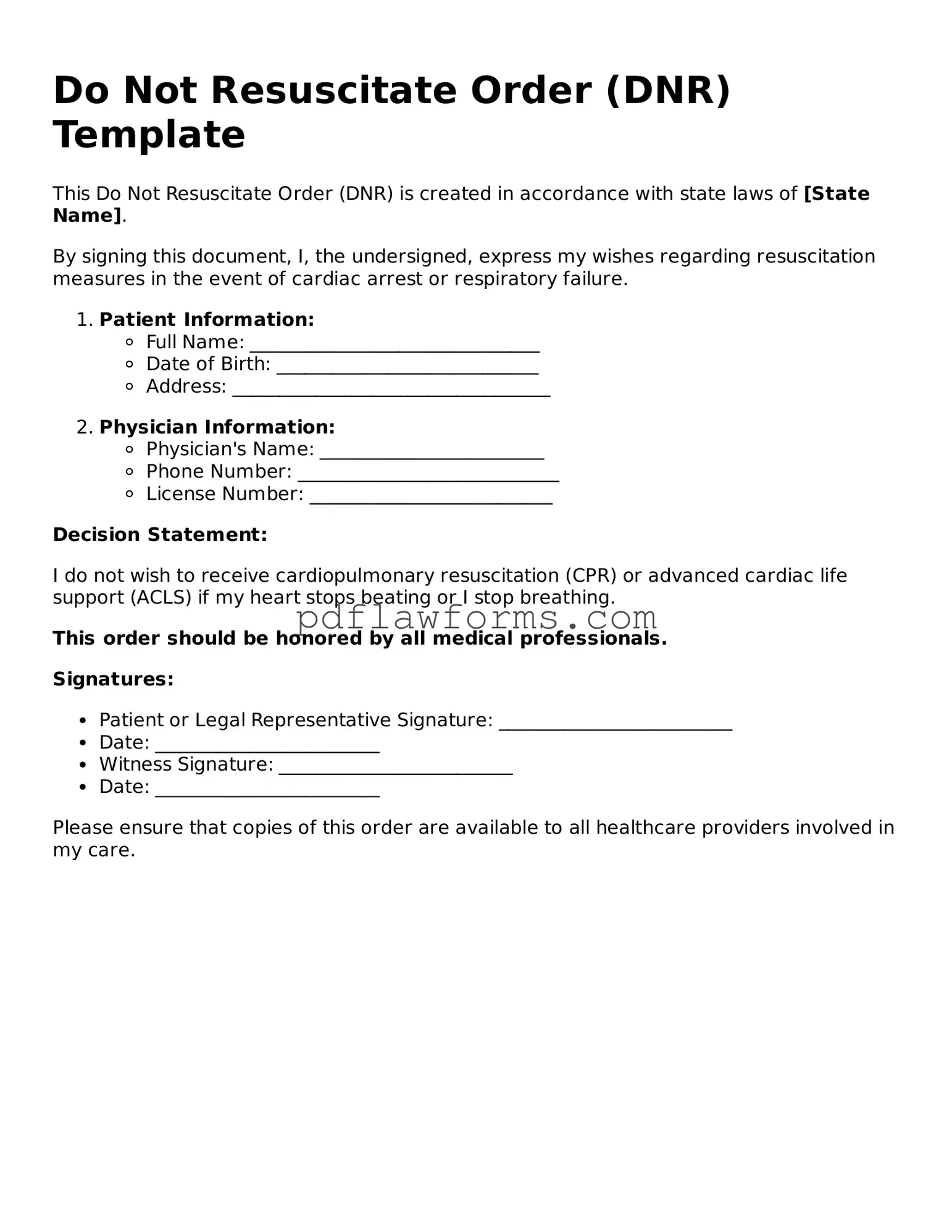
Official Do Not Resuscitate Order Form
A Do Not Resuscitate (DNR) Order is a legal document that allows individuals to express their wishes regarding resuscitation efforts in the event of a medical emergency. By completing this form, you ensure that your preferences are respected and followed by healthcare providers. To take control of your healthcare decisions, consider filling out the DNR Order form by clicking the button below.
Make My Document Online
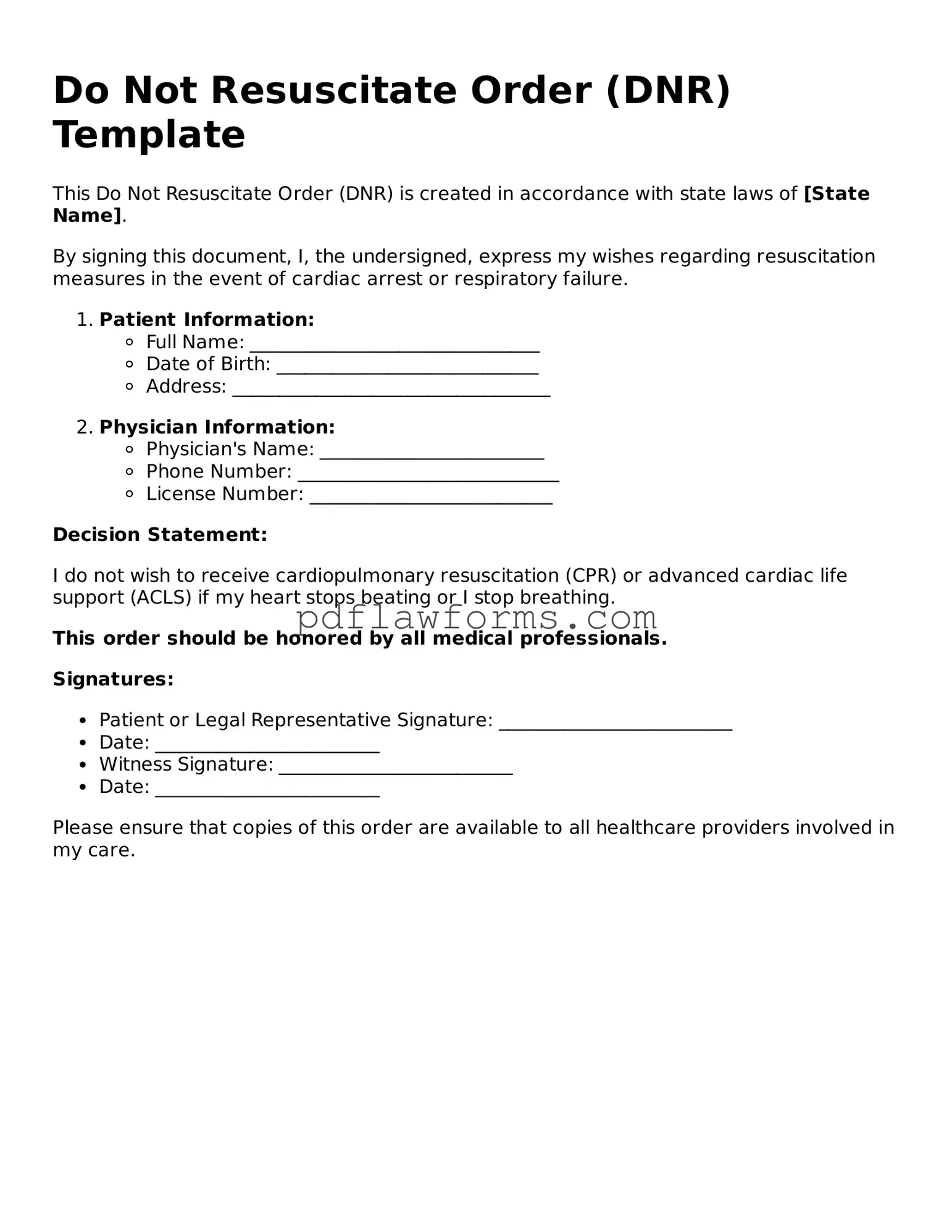
Official Do Not Resuscitate Order Form
Make My Document Online
You’re halfway through — finish the form
Edit and complete Do Not Resuscitate Order online, then download your file.
Make My Document Online
or
⇩ Do Not Resuscitate Order PDF